PATIENT INFORMATION
CPAP Alternatives
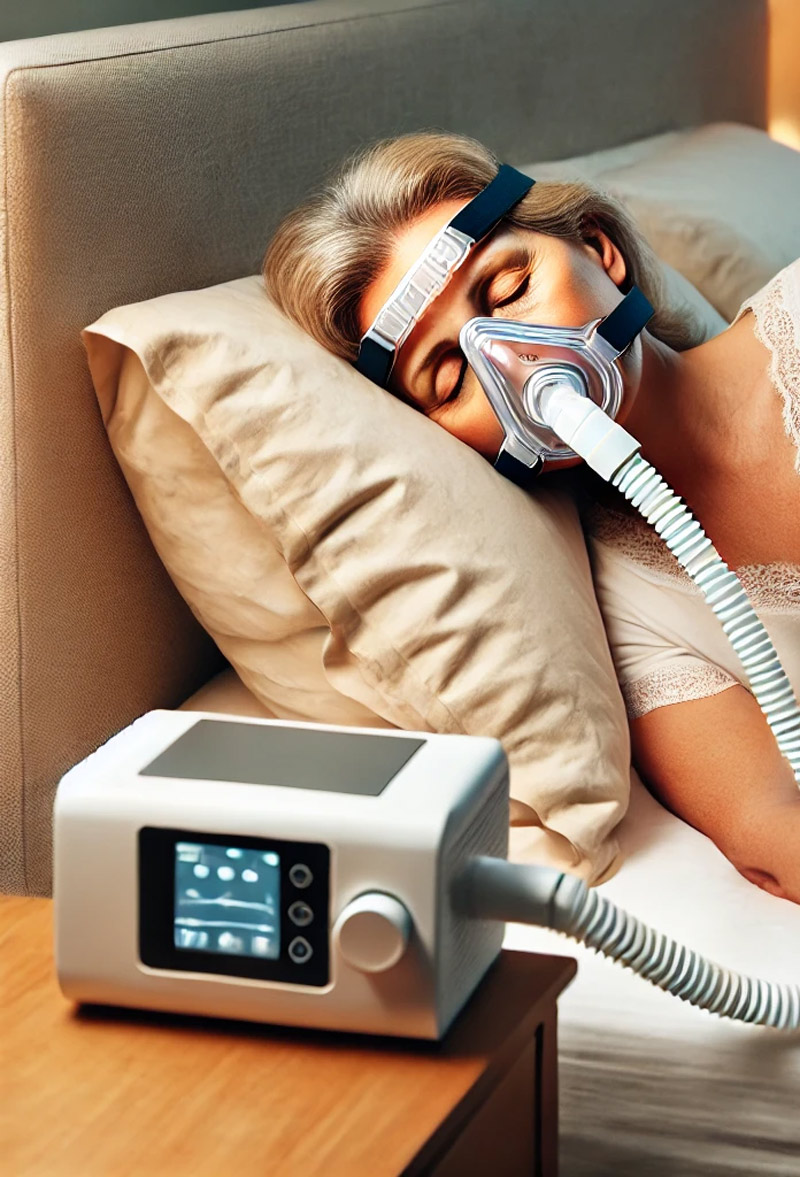
Many people assume that the go-to solution for Obstructive Sleep Apnea is an uncomfortable CPAP machine. CPAP stands for Continuous Positive Airway Pressure. The machine is attached to a mask you wear to bed that covers your nose and/or your mouth and pushes in a stream of air to keep your airway open while you sleep.
We’ve helped thousands of patients achieve better sleep thru Oral Appliance Therapy without the drawbacks of CPAP machines. Make sure to talk to your doctor about the potential of this type of treatment when considering alternatives.
CPAP Machine Overview
About 30 million people in the United States likely have Obstructive Sleep Apnea (OSA), but only 6 million are diagnosed with the condition. If you’ve noticed things like irregular breathing at night, waking up gasping for air, or feeling exhausted during the day, it’s worth a chat with your doctor who can help figure out if you’re at risk. Leaving OSA untreated can lead to serious health issues, like high blood pressure, heart rhythm problems, depression, and strokes. OSA has also been linked to car accidents and injuries at work due to exhaustion.
Many people assume that the go-to solution for OSA is a CPAP machine. CPAP stands for Continuous Positive Airway Pressure. The machine is attached to a mask you wear to bed that covers your nose and/or your mouth and pushes in a stream of air to keep your airway open while you sleep.

High Rates of CPAP Abandonment
The severity of sleep apnea is measured using the Apnea-Hypopnea Index (AHI), which tracks how many breathing pauses (apneas) occur per hour.
| AHI | Severity |
|---|---|
| <5 | Normal Sleep |
| 5-14 | Mild OSA |
| 15-29 | Moderate OSA |
| >30 | Severe OSA |
The goal of CPAP therapy is to reduce your AHI to a level below 5. This is clearly a vast improvement for someone with severe or even moderate OSA – if they stick with it. You may have heard that CPAP treatment is uncomfortable, noisy, dries out your mouth, and may fall off when you toss and turn in your sleep. They can also be cumbersome to travel with.
While it’s highly effective in treating OSA, the CPAP treatment is abandoned by about 38% of the patients for these very reasons.
In truth, a CPAP machine may be overkill, especially for some cases of mild to moderate OSA. There are other ways to tackle sleep apnea. In this article we’ll explore some of the other options that might be easier, less intrusive and more comfortable solutions than a CPAP machine.
While it is highly effective in treating OSA, CPAP treatment is abandoned by about 38% of patients.
Oral Appliances: The Simple Alternative to CPAP
For many people, oral appliances, also called Mandibular Advancement Devices (MADs) are very effective treatments for sleep apnea. These devices are much smaller and more comfortable than CPAP machines, making them a great alternative for people who don’t like the idea of wearing a noisy mask to bed.
Mandibular Advancement Devices (MADs) are a great choice for treating OSA because they’re comfortable and effective. These devices work by gently repositioning your lower jaw forward, which in turn moves your tongue away from your airway, keeping it open while you sleep.


The goal is to prevent the airway blockages that happen with sleep apnea, so you can breathe more freely throughout the night. What’s great about MADs is that they’re custom-made so they’re designed to fit your mouth perfectly. This personalized fit means you’re less likely to experience discomfort, and they typically don’t interfere with your bite. The devices are small and easy to wear.
Many people find them to be much more comfortable than using a CPAP machine.
Plus, they’re discreet, so no one will know you’re wearing them while you sleep. MADs have been shown to reduce both snoring and sleep apnea symptoms, and for many people, they can be a great first step before even considering other treatments. They’re a non-invasive, low-maintenance option that can significantly improve your sleep quality without the need for bulky equipment.
Many people find wearing an oral appliance to be much more comfortable and just as effective as using a CPAP machine.
Positional Therapy
Don’t Sleep on Your Back
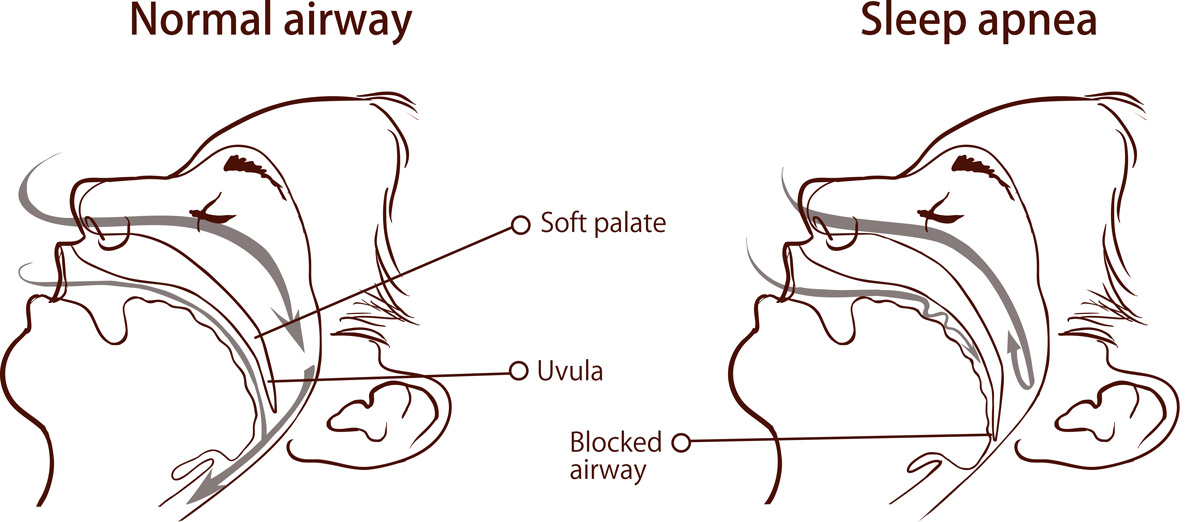
Obstructive sleep apnea (OSA) occurs when the muscles in your throat relax too much during sleep, causing your airway to narrow or close completely. OSA is worse when you sleep on your back. This condition is known as positional sleep apnea (POSA).
When you lie on your back gravity causes your tongue and soft tissues to collapse backward, blocking your airway.Positional therapy is a possible solution that helps keep you on your side while you sleep, where your airway stays more open.
Here are some ways that Positional Therapy is applied:
Special pillows: These have “sleeves” for your arms and are generally designed to make side sleeping more comfortable and natural.
Back-position blockers: Placing something uncomfortable (like a tennis ball or wiffle ball) in a back pocket or a “backpack”, or stitched to the back of a t-shirt, keeps you from rolling over during the night.
Wearable alarms: These buzz or vibrate when you roll onto your back, gently reminding you to switch positions.


Research shows positional therapy may reduce apnea episodes for people whose symptoms are worse on their backs. It can decrease AHI by 7 events per hour. Although it isn’t as effective at reducing AHI as CPAP many people find positional therapy easier to stick with, using it for an average of 2.5 hours longer per night.
If your OSA symptoms are mild to moderate and worsen when you sleep on your back, positional therapy might be a great option. It’s a non-invasive and relatively low-cost solution that could help improve your sleep and overall quality of life.
That said, it’s not perfect. Some people find the devices uncomfortable and report mild side effects, such as sleep disturbances or back and chest discomfort. But if you’re willing to give it a try, positional therapy is a non-invasive, low-cost option that just might make a big difference in how you sleep—and feel—every day.
MyoFunctional Therapy
Strengthening Your Facial and Tongue Muscles
Myofunctional therapy is a structured exercise program designed to train and strengthen the muscles around your face, mouth, and tongue. It’s a non-invasive treatment (or exercise regimen) that can improve issues related to breathing and snoring.
This therapy targets orofacial myofunctional disorders (OMDs)—abnormal patterns of movement in the face and mouth. These can stem from a variety of causes, such as:
– Blocked nasal passages.
– Tongue positioning issues.
– Persistent thumb sucking or chewing habits in adults.
Through neuromuscular exercises, myofunctional therapy aims to restore proper muscle function.
A certified myofunctional therapist will assess your specific needs and develop a tailored exercise program that may include tongue presses, balloon breathing, cheep and lip exercises and specific swallowing techniques that help retrain the way your tongue and throat muscles work
While research is ongoing, evidence supports myofunctional therapy as a valuable tool in managing sleep-disordered breathing, either on its own or alongside other treatments.
If you’re looking for a non-invasive, low-cost way to improve your breathing and sleep quality, myofunctional therapy is worth considering. Speak with a specialist to find out if it’s right for you.
Weight Loss and Lifestyle Changes
Obesity is a major risk factor for sleep apnea. Losing weight through diet and exercise has been shown to improve, and sometimes largely resolve, sleep apnea symptoms.
Combining weight loss with positional therapy or other treatments can yield even better results. Avoiding alcohol, which relaxes throat muscles and worsens OSA, is another simple yet effective step.
Small changes in your daily habits can go a long way toward improving sleep apnea symptoms. While these strategies aren’t a replacement for medical treatments like CPAP, they can complement your care and help you sleep better:
Lose Weight: Shedding extra pounds might not completely cure OSA, but it can reduce the number of breathing interruptions during sleep. In some cases, doctors may recommend weight-loss surgery for significant results.
Get Moving: Regular exercise can improve your sleep apnea, even if it doesn’t lead to visible weight loss. A simple daily walk or workout can make a difference.
Skip the Nightcap: Alcohol and sedatives relax throat muscles, making OSA worse. Try avoiding them, especially before bed.
Cut Out Irritants: For allergen-sensitive people and especially for children with OSA, reducing allergens, smoke, or irritants in their sleeping space can help them breathe easier at night.

Myofunctional therapy, positional therapy, and lifestyle changes can all help improve sleep apnea symptoms.

Surgery
Reshaping Your Airway
Sometimes, your anatomy is the main culprit. Large tonsils, a floppy soft palate, or a jaw structure that’s too small can all contribute to sleep apnea. Depending on the issue and severity of your OSA, surgery may be something to discuss with your doctor.
Surgery isn’t usually the first choice, but it might be an option if you have a clearly correctable physical problem like enlarged tonsils or a floppy soft palate. The goal is to remove or reshape tissues in your airway to reduce blockages during sleep. One of the most common procedures is Uvulopalatopharyngoplasty (or UPPP).
This involves removing or repositioning tissue around the upper airway. In certain cases, maxillomandibular advancement may be recommended, which involves repositioning the upper and lower jaw to create more space in the airway. For children with enlarged tonsils and adenoids, a tonsillectomy often resolves most OSA symptoms.
Another surgical procedure that has been approved by the FDA for treatment of moderate to severe OSA is hypoglossal nerve stimulation. HNS is a relatively new treatment for obstructive sleep apnea. This implantable device gently stimulates a nerve under your tongue to keep your airway open while you sleep, reducing snoring, gasping, and choking. It’s kind of like a pacemaker for the hypoglossal nerve.
The implant surgery is an outpatient procedure lasting 2–3 hours under general anesthesia and includes a breathing sensor placed near your ribs to monitor your breathing, a pulse generator implanted in your chest to send electrical signals, and an electrode cuff around the hypoglossal nerve that moves your tongue forward to clear your airway. A handheld remote controls the device, allowing you to turn it on and off or delay activation until after you’ve fallen asleep.
For people with moderate to severe sleep apnea (AHI score of 15–65) who cannot tolerate CPAP and have tried and were not helped by alternatives, this treatment may be a promising option. Talk to your medical professional to see if the possible side effects are worth it.
Emerging Treatments
High Tech Possible Alternatives
Research into new solutions for sleep apnea continues. Medications and other non-invasive options may soon offer additional choices for managing the condition.
If you’re looking for alternatives to the traditional CPAP machine for treating sleep apnea, there are some emerging options that might work for you. One of these is Continuous Negative External Pressure (cNEP), which works differently from the CPAP.
Instead of forcing air into your airways, cNEP uses a silicone collar that applies gentle negative pressure around the neck and pulls the tissues of the throat to keep the airway open. This can improve airflow during sleep. For people who find CPAP masks uncomfortable or difficult to tolerate, cNEP offers a maskless approach.
Another option gaining traction is Oral Pressure Therapy. OPT uses a specially designed mouthpiece that creates suction to help keep the airway open during sleep. It’s a more discreet option compared to CPAP and doesn’t involve the bulky mask or the noise that many users find annoying.
This therapy can be especially helpful for those with mild to moderate obstructive sleep apnea. It works by gently pulling the soft tissues of the throat forward, which helps prevent airway collapse. Some people find OPT to be a more comfortable and effective alternative.
Both cNEP and OPT offer promising solutions for those who struggle with traditional CPAP treatment.

Consult with your doctor about your specific needs and the best option for treatment for your sleep apnea.
Conclusion
The best option for treating sleep apnea always depends on your specific needs and the severity of your condition. It’s always a good idea to consult with your doctor to explore which treatment might be most effective for you.
As sleep apnea treatments continue to evolve, it’s reassuring to know there are choices available that can help improve your quality of sleep – and thus your overall health – without the drawbacks of traditional CPAP machines.
We’ve helped thousands of patients achieve better sleep thru Oral Appliance Therapy without the drawbacks of CPAP machines. Make sure to talk to your doctor about the potential of this type of treatment when considering alternatives.

We’ve helped thousands of patients achieve better sleep without the drawbacks of CPAP machines.
